How long should a person stay awake after a head injury? It’s a question that holds the key to a crucial aspect of recovery. The period of wakefulness immediately following a head injury can significantly impact the healing process and cognitive restoration. In this article, we uncover the science behind post-injury rest and explore the guidelines that medical experts recommend for optimal recovery.
In short, the duration of wakefulness after a head injury is a critical factor that shouldn’t be overlooked. Rest is not just about getting some shut-eye; it directly influences how the brain heals and restores its functions. Following the right wakefulness period can make all the difference in a successful recovery.
As you read further, we will delve into the importance of sleep in brain recovery and how different factors, such as the severity of the injury and individual characteristics, play a role in determining the ideal wakefulness duration. We’ll also discuss the medical guidelines and explore real-life case studies to illustrate the impact of adhering to these recommendations. If you or someone you know has experienced a head injury, understanding the significance of post-injury rest is crucial for a successful healing journey. Let’s embark on this exploration together and discover the optimal path to a healthier brain.
Remember, recovery is not just about physical healing; it’s about giving your brain the rest it needs to bounce back stronger. So, without further ado, let’s dive into the fascinating world of post-head injury wakefulness and its impact on the miraculous human brain!
Understanding Head Injuries and their Impact on the Brain
In this section, we delve into the intricate world of head injuries and their profound impact on the brain. Defined as any trauma or damage to the head region, head injuries encompass a variety of types, including concussions, contusions, and more. Each type brings its own set of challenges and potential consequences, underscoring the importance of understanding these injuries to better navigate their aftermath.
The mechanism of injury lies at the heart of comprehending the repercussions on the brain. When the head suffers a blow or experiences a sudden jolt, the brain can collide with the inner skull, leading to potential bruising or bleeding. This disruption can cause a chain reaction of events that affect the brain’s delicate functionality. As the epicenter of the central nervous system, the brain controls every aspect of our being, making any injury to this vital organ a matter of utmost concern.
Immediate effects of head injuries manifest in various ways, with wakefulness and cognitive function being particularly impacted. Individuals who have experienced head trauma often report feeling disoriented or dazed, and in more severe cases, may lose consciousness altogether. These effects can be alarming and, in some cases, require immediate medical attention. Additionally, cognitive function can suffer, leading to memory lapses, difficulty concentrating, and impaired decision-making abilities. Such cognitive challenges can be distressing and frustrating, making it crucial for individuals to seek prompt medical evaluation and support.
When it comes to head injuries, time is of the essence. Swift identification and appropriate response are paramount in mitigating potential complications and promoting the best chance of recovery. Properly diagnosing the type of head injury is essential, as treatment approaches may differ based on the specific condition. For instance, a concussion may necessitate rest and a gradual return to normal activities, while a more severe contusion may require surgery or other medical interventions.
To optimize recovery outcomes, a multi-faceted approach is vital. Medical professionals, including neurologists and neurosurgeons, play a pivotal role in evaluating head injuries and providing tailored treatment plans. Additionally, monitoring wakefulness and cognitive function during the recovery phase can offer critical insights into the brain’s healing progress. Family members and caregivers also play a crucial role in supporting the individual’s well-being during this period, providing emotional and physical assistance as needed.
As we navigate the complex terrain of head injuries and their impact on the brain, it is essential to recognize the importance of post-injury rest. Adequate rest allows the brain the time and space it needs to heal and regain its cognitive functions. Following medical guidelines and adhering to prescribed periods of wakefulness can significantly influence the trajectory of recovery. However, individual factors, such as age, overall health, and the severity of the injury, must also be considered when determining the optimal duration of wakefulness.
Furthermore, advancements in medical research continue to shed light on the intricate workings of the brain and its resilience in the face of injury. By staying abreast of the latest scientific findings, medical professionals can fine-tune treatment strategies and optimize outcomes for patients recovering from head injuries.
The Role of Sleep in Brain Recovery
When it comes to the intricate process of brain recovery, sleep emerges as a true hero, playing a pivotal role in healing and tissue repair. Beyond its restorative benefits for the body, sleep is a dynamic process that actively contributes to the rejuvenation of cognitive functions and overall brain health. Let’s explore the profound importance of sleep in the brain’s recovery journey, unraveling the fascinating world of slumber and its impact on our most vital organ.
Healing and Tissue Repair: Sleep acts as a powerful catalyst for brain healing and tissue repair. During sleep, the brain engages in intricate mechanisms that facilitate the repair of damaged cells and tissues. Growth hormone production peaks during deep sleep, promoting cellular regeneration and restoring vital brain structures. Furthermore, sleep offers the brain a crucial window of time to remove toxins and metabolic waste, fostering a clean slate for optimal functioning.
The Stages of Sleep and Their Significance: Sleep is not a monolithic process but is characterized by distinct stages, each with its unique contribution to brain recovery. The sleep cycle encompasses two main categories: Rapid Eye Movement (REM) sleep and Non-Rapid Eye Movement (NREM) sleep. NREM sleep is further divided into three stages:
NREM Stage 1: This is the transitional phase between wakefulness and sleep, a brief period lasting a few minutes. Brainwave patterns start to slow down, preparing the brain for deeper slumber.
NREM Stage 2: In this stage, the brain enters a light sleep characterized by sleep spindles and K-complexes. The body temperature decreases, and heart rate and breathing become regular.
NREM Stage 3 (Deep Sleep): Also known as slow-wave sleep, this stage is critical for physical restoration and memory consolidation. During deep sleep, the brain undergoes significant repair processes, and growth hormone secretion reaches its peak.
REM Sleep: This is the stage where most dreaming occurs. REM sleep is essential for emotional processing and memory consolidation, allowing the brain to integrate new information and experiences into existing neural networks.
Brain Activity During Sleep and Cognitive Restoration: Contrary to popular belief, the brain remains remarkably active during sleep, engaging in a symphony of complex activities that contribute to cognitive restoration. During REM sleep, the brain forms new neural connections and strengthens existing ones, enhancing learning and memory retention. Additionally, REM sleep plays a crucial role in emotional regulation and creative problem-solving. The brain’s ability to process emotions and experiences during REM sleep contributes to emotional well-being and psychological resilience.
As we unlock the secrets of sleep’s role in brain recovery, it becomes evident that optimizing sleep quality and duration is paramount for overall well-being. Adequate and restful sleep serves as a natural balm for the brain, promoting its healing and restoration after injury or trauma. However, achieving optimal sleep can be challenging, especially for those recovering from head injuries. Patients and caregivers must prioritize sleep hygiene and create an environment conducive to restful slumber.
Creating a sleep-friendly environment involves simple yet effective strategies, such as maintaining a consistent sleep schedule, avoiding stimulants before bedtime, and limiting screen time before sleep. Moreover, implementing relaxation techniques, such as meditation and deep breathing exercises, can further aid in promoting deep and restorative sleep.
Factors Influencing Wakefulness Duration
When it comes to determining the duration of wakefulness after a head injury, a myriad of factors come into play, each holding a unique influence on the recovery process. From individual characteristics to the nature of the head injury itself, a comprehensive understanding of these factors is crucial in tailoring the most appropriate wakefulness period for optimal healing and cognitive restoration.
Individual Factors: Age, overall health, and medical history are key individual factors that significantly impact wakefulness duration. The body’s ability to heal and recover varies across different age groups. Younger individuals tend to bounce back more quickly due to their robust regenerative capacity, while older adults may require more time to recover fully. Moreover, an individual’s overall health plays a vital role in determining their resilience to head injuries. Pre-existing medical conditions or compromised immune systems may necessitate an extended wakefulness period to facilitate recovery. Medical history also sheds light on any previous head injuries or neurological conditions that may influence the current wakefulness recommendations.
Severity of the Head Injury: The severity of the head injury itself is a critical determinant of the recommended wakefulness duration. Mild concussions may require a relatively shorter wakefulness period, whereas more severe injuries, such as traumatic brain injuries (TBIs), demand longer periods of wakefulness to monitor for potential complications. Medical professionals carefully assess the extent of the injury, employing diagnostic tools such as brain imaging and neurological examinations to gauge the severity accurately. The severity of the injury directly correlates with the potential risks and challenges in the recovery process, guiding medical practitioners in devising the most suitable wakefulness protocols.
Role of Medical Treatment and Interventions: Medical treatment and interventions significantly influence the appropriate duration of wakefulness after a head injury. Prompt medical evaluation and intervention are critical in managing head injuries effectively. In some cases, surgical interventions may be required to address intracranial bleeding or other severe complications. Following such procedures, the wakefulness period may be extended to closely monitor the patient’s condition and ensure timely detection of any post-operative complications. Moreover, medical treatments, such as medications to control intracranial pressure or manage pain, may also influence the wakefulness duration as patients need to be observed during their effects on cognitive function.
The Role of Multidisciplinary Collaboration: Managing the wakefulness duration after a head injury requires a collaborative approach involving multiple medical specialties. Neurologists, neurosurgeons, intensive care specialists, and other healthcare professionals work together to assess the patient’s condition comprehensively. The expertise and insights from each specialty contribute to a well-rounded understanding of the patient’s needs, enabling the development of a tailored wakefulness plan that accounts for the various factors influencing recovery.
In conclusion, determining the optimal wakefulness duration after a head injury involves a delicate balancing act, taking into account various individual factors, the severity of the injury, and the role of medical treatments and interventions. Multidisciplinary collaboration is the bedrock of providing comprehensive care to patients recovering from head injuries, ensuring that no aspect of the recovery journey is overlooked. By tailoring wakefulness protocols to suit each individual’s unique circumstances, medical practitioners pave the way for enhanced brain healing and cognitive restoration. Ultimately, the synergy between medical expertise and personalized care lies at the heart of unlocking the full potential of the brain’s remarkable capacity to heal and recover from head injuries.
Medical Guidelines for Wakefulness After Head Injury
Navigating the path to recovery after a head injury requires adherence to well-established medical guidelines and recommendations. These guidelines serve as beacons of light, guiding healthcare professionals in providing the most effective care to patients. In this section, we shed light on the existing medical guidelines for post-injury wakefulness, uncovering the rationale behind them, and delving into the scientific evidence supporting their significance.
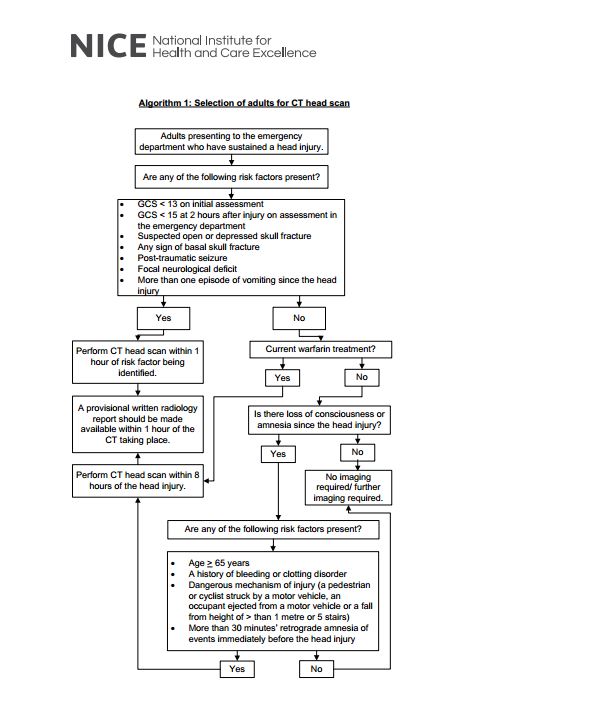
Presenting the Existing Medical Guidelines: Medical guidelines for wakefulness after a head injury emphasize the critical importance of monitoring patients closely during the initial period following the trauma. These guidelines advocate for periods of wakefulness and observation, often spanning a few hours to a day, depending on the severity of the injury. During this time, healthcare professionals diligently assess the patient’s cognitive function, neurological responses, and signs of potential complications. The decision to recommend wakefulness is grounded in the desire to promptly detect any red flags that may warrant further medical intervention.
The Rationale Behind the Guidelines: The rationale behind the recommended wakefulness duration lies in the nature of head injuries and their potential to manifest symptoms and complications gradually. Concussions, for example, may not immediately present obvious symptoms, leading to a phenomenon known as “silent concussions.” By closely monitoring patients during the wakefulness period, medical professionals can promptly identify any emerging symptoms or signs of deterioration that may necessitate immediate intervention. Early detection allows for timely medical care, significantly improving the chances of successful recovery and reducing the risk of long-term complications.
Scientific Evidence Supporting Wakefulness Duration: The scientific evidence supporting the medical guidelines for wakefulness after head injury is rooted in a wealth of research and clinical studies. Numerous studies have highlighted the importance of close monitoring during the initial period following head trauma. Research shows that individuals with head injuries who are observed for an extended period tend to have better outcomes compared to those with delayed intervention. Furthermore, studies examining the effects of wakefulness on cognitive recovery indicate that early detection and management of potential complications positively impact brain healing and cognitive function restoration.
Addressing Controversies and Conflicting Viewpoints: While medical guidelines advocate for periods of wakefulness, some controversies and conflicting viewpoints exist within the medical community. Some experts argue that prolonged wakefulness may lead to unnecessary stress and fatigue in patients, potentially hindering the recovery process. These conflicting viewpoints highlight the need for individualized care and careful consideration of each patient’s unique circumstances. In some cases, healthcare professionals may opt for shorter wakefulness periods, depending on the patient’s overall health, medical history, and specific injury characteristics.
Monitoring and Assessing Cognitive Function
During the wakefulness period after a head injury, monitoring cognitive function is of paramount importance, as it provides crucial insights into the brain’s healing progress and guides medical decisions. Understanding the significance of monitoring cognitive abilities, the methods employed for assessment, and recognizing signs that may indicate the need for prolonged rest or medical intervention is essential for ensuring optimal recovery and well-being.
1. The Importance of Monitoring Cognitive Function: Cognitive function encompasses a wide array of mental processes, including memory, attention, language, and problem-solving. Monitoring these abilities during the wakefulness period allows medical professionals to gauge the brain’s response to the injury and detect any cognitive impairments or changes that may require attention. Timely identification of cognitive challenges can prompt targeted interventions, fostering better outcomes and reducing the risk of long-term cognitive deficits.
2. Methods and Tools for Cognitive Assessment: Various methods and tools are used to assess cognitive abilities and track changes over time. Some common approaches include:
Neurological Examination: This involves a comprehensive assessment of neurological functions, including tests for reflexes, sensory perception, and motor skills.
Cognitive Tests: Standardized cognitive tests assess specific aspects of cognitive function, such as memory, attention, and executive functions. Examples include the Montreal Cognitive Assessment (MoCA) and the Mini-Mental State Examination (MMSE).
Imaging Studies: Brain imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), offer valuable insights into the brain’s structural integrity and aid in identifying areas of injury or abnormalities.
Neuropsychological Evaluation: Conducted by trained neuropsychologists, this evaluation provides an in-depth analysis of cognitive abilities and helps identify subtle changes that may not be evident in standard cognitive tests.
3. Signs Indicating the Need for Prolonged Rest or Medical Intervention: Several signs may indicate the necessity for extended rest or medical attention during the wakefulness period:
Persistent Headaches: Frequent or severe headaches may signal complications, such as increased intracranial pressure, requiring medical evaluation.
Nausea and Vomiting: These symptoms may indicate underlying issues that warrant further investigation.
Disorientation and Confusion: Persistent disorientation or confusion may point to ongoing cognitive challenges that need to be addressed.
Worsening Cognitive Function: A decline in cognitive abilities or the emergence of new cognitive difficulties may necessitate extended monitoring and intervention.
Unconsciousness: Prolonged or recurrent unconsciousness warrants immediate medical attention to assess the severity of the injury and potential brain damage.
It is important to note that each individual’s response to a head injury may vary, and the need for prolonged rest or medical intervention should be determined on a case-by-case basis, considering factors such as age, overall health, and the nature of the head injury.
Recognizing and Managing Complications
In the realm of head injury recovery, recognizing and managing potential complications arising from insufficient or excessive wakefulness is of paramount importance in ensuring optimal patient outcomes. As medical professionals diligently monitor patients during the wakefulness period, they must remain vigilant for any signs of complications that may warrant prompt intervention. By understanding these potential challenges and employing effective management strategies, healthcare providers can navigate the complexities of head injury recovery with precision and care.
Identifying Potential Complications:
Delayed Detection of Underlying Injuries: Insufficient wakefulness may result in delayed detection of underlying injuries, particularly those with subtle symptoms. Such delayed detection can lead to the exacerbation of injuries and hinder the timely initiation of appropriate treatments.
Exacerbation of Cognitive Deficits: Prolonged wakefulness without adequate rest may exacerbate cognitive deficits, impairing memory, attention, and problem-solving abilities. This can hinder the recovery process and affect an individual’s overall quality of life.
Increased Risk of Secondary Injuries: Insufficient wakefulness can increase the risk of secondary injuries, especially in cases where patients engage in activities beyond their cognitive capacity during the recovery period.
Complications from Excessive Wakefulness: Conversely, excessive wakefulness without appropriate rest can lead to increased stress and fatigue, potentially hindering the brain’s healing process.
Strategies and Interventions for Effective Management:
Individualized Care Plans: Tailoring care plans to each patient’s unique circumstances is essential in managing complications effectively. Personalized care accounts for factors such as age, overall health, severity of the head injury, and response to treatments.
Cognitive Rehabilitation: For individuals experiencing cognitive deficits, cognitive rehabilitation programs offer targeted interventions to improve cognitive function, memory, and attention. These programs involve various exercises and techniques to stimulate brain plasticity and enhance cognitive abilities.
Rest and Gradual Reintegration: Striking the right balance between wakefulness and rest is critical in managing complications. Gradually reintegrating patients into daily activities based on their cognitive progress helps prevent overexertion and supports their overall recovery.
Multidisciplinary Collaboration: Effective management of complications necessitates a multidisciplinary approach. Collaborative efforts involving neurologists, neuropsychologists, physical therapists, and other specialists contribute to a comprehensive understanding of the patient’s needs and enable targeted interventions.
Education and Support: Providing patients and their families with education and support is vital in managing complications and promoting patient well-being. Educating them about potential challenges, warning signs, and strategies for managing cognitive deficits empowers them to take an active role in the recovery process.
Medication Management: In cases where complications arise from specific medical issues, appropriate medication management can alleviate symptoms and support the healing process. Healthcare professionals carefully consider the risks and benefits of medications, tailoring treatments to individual needs.
Adherence to Follow-Up Care: Encouraging patients to adhere to follow-up care appointments ensures that any emerging complications are detected and addressed promptly. Regular assessments and adjustments to the care plan help optimize recovery outcomes.
Case Studies and Real-Life Examples
The impact of head injuries on individuals can vary significantly based on the duration of wakefulness and adherence to medical guidelines during the crucial recovery period. Real-life case studies offer valuable insights into the outcomes experienced by individuals who have suffered head injuries, shedding light on the significance of managing wakefulness effectively for better recovery prospects.
1. Case Study 1 – Insufficient Wakefulness:
Patient Profile: A 35-year-old individual experienced a mild head injury after a fall. However, due to a lack of awareness regarding the importance of wakefulness, the patient resumed regular activities soon after the incident without adequate rest.
Outcome: The patient initially reported minor headaches and difficulties concentrating but attributed them to stress. As days passed, the cognitive challenges worsened, impacting work performance and daily activities. Eventually, the patient sought medical attention, revealing underlying cognitive deficits that required targeted cognitive rehabilitation.
Analysis: The case highlights the potential consequences of insufficient wakefulness, as the patient’s cognitive deficits worsened due to the lack of early intervention. Adherence to medical guidelines for post-injury wakefulness could have prompted early detection and management, potentially mitigating cognitive impairments.
2. Case Study 2 – Adherence to Medical Guidelines:
Patient Profile: A 21-year-old athlete sustained a moderate head injury during a sporting event. Recognizing the importance of wakefulness, the patient followed medical guidelines, adhering to the recommended wakefulness period and closely monitoring any changes.
Outcome: The patient experienced mild headaches and cognitive difficulties during the wakefulness period but refrained from engaging in mentally taxing activities. With sufficient rest and adherence to guidelines, the cognitive challenges gradually improved, and the patient returned to regular activities with no lasting impairments.
Analysis: This case illustrates the positive impact of adhering to medical guidelines for wakefulness after a head injury. By closely monitoring cognitive function and avoiding activities that could exacerbate the injury, the patient achieved a successful recovery with minimal long-term consequences.
3. Case Study 3 – Excessive Wakefulness:
Patient Profile: A 50-year-old individual suffered a severe head injury in a car accident and was hospitalized for observation. The patient experienced restlessness and anxiety, leading to excessive wakefulness despite medical recommendations.
Outcome: The patient’s excessive wakefulness led to increased stress and agitation, affecting the body’s ability to heal. Cognitive assessments indicated significant impairments that required intensive cognitive rehabilitation and extended hospitalization.
Analysis: This case emphasizes the adverse effects of excessive wakefulness, as it impeded the brain’s healing process and exacerbated cognitive deficits. Proper management of wakefulness through rest and gradual reintegration into activities could have supported the brain’s recovery more effectively.
4. Case Study 4 – Individualized Care Plan:
Patient Profile: A 65-year-old individual suffered a head injury from a fall, but the severity of the injury was unclear initially. Medical professionals tailored an individualized care plan based on the patient’s medical history and age.
Outcome: The patient underwent thorough neurological examinations and cognitive assessments during the wakefulness period. Based on the findings, a personalized cognitive rehabilitation program was designed, leading to significant improvements in cognitive function.
Analysis: This case underscores the importance of individualized care plans in managing head injury complications. By considering the patient’s unique circumstances and response to treatments, healthcare providers optimize the chances of successful recovery.
Tips for Optimal Brain Recovery

Recovering from a head injury can be a challenging journey, but with the right strategies and lifestyle adjustments, individuals can optimize their brain recovery and foster a smoother path to healing. Whether dealing with mild or severe head trauma, incorporating practical tips and advice into the recovery process can make a significant difference in the overall outcome. Here are some essential tips to aid in the recovery process and promote optimal brain health:
1. Prioritize Rest and Sleep Hygiene:
- Ensure sufficient sleep each night, aiming for 7-9 hours of restful sleep.
- Create a calming sleep environment by minimizing noise and light distractions.
- Establish a consistent sleep schedule to regulate the body’s natural sleep-wake cycle.
2. Gradual Return to Activities:
- Gradually reintroduce daily activities based on cognitive progress and medical guidance.
- Avoid engaging in mentally taxing or physically demanding tasks during the initial recovery phase.
3. Follow Medical Guidelines:
- Adhere to medical recommendations for the duration of wakefulness after the head injury.
- Attend follow-up appointments and assessments to monitor progress and adjust the care plan accordingly.
4. Incorporate Brain-Boosting Foods:
- Consume a balanced diet rich in brain-boosting nutrients such as omega-3 fatty acids, antioxidants, and vitamins.
- Include foods like fatty fish, nuts, seeds, leafy greens, and colorful fruits to support brain health.
5. Stay Hydrated:
- Maintain proper hydration to support overall brain function and prevent dehydration-related complications.
- Drink water regularly throughout the day, especially during warmer weather or physical activities.
6. Engage in Mental Exercises:
- Stimulate the brain with mental exercises such as puzzles, crosswords, or memory games.
- Reading, learning a new skill, or engaging in creative activities can also enhance cognitive function.
7. Seek Emotional Support:
- Reach out to friends, family, or support groups to share feelings and experiences during the recovery process.
- Emotional support can provide encouragement and help manage stress and anxiety.
8. Avoid Substance Abuse:
- Refrain from alcohol consumption and avoid recreational drug use, as these can impede the brain’s healing process.
- Consult with healthcare professionals about any prescribed medications and their potential interactions.
9. Stay Active with Low-Impact Exercises:
- Engage in low-impact exercises like walking, yoga, or swimming, which can promote blood flow to the brain without straining the body.
- Physical activity can also boost mood and overall well-being during the recovery period.
10. Manage Stress:
- Practice stress-reduction techniques such as deep breathing, meditation, or mindfulness exercises.
- Managing stress supports the healing process and helps prevent unnecessary strain on the brain.
11. Collaborate with Healthcare Providers:
- Work closely with healthcare professionals to create an individualized care plan that meets specific recovery needs.
- Regularly communicate any changes in symptoms or concerns to ensure proper management.
Key points
It is critical to consider the duration of wakefulness after a head injury in order to successfully recover. Sleep plays an important role in brain healing and tissue regeneration, so it is critical to follow medical recommendations for optimal rest. Understanding the factors that influence wakefulness duration and cognitive function during the recovery phase can help people take proactive steps to support their brain’s recovery.
The recommendation for wakefulness after a head injury is not a one-size-fits-all approach. In addition to the severity of the injury, the victim’s age, overall health, and individual characteristics must be considered. While medical guidelines can be useful reference points, one must always consult a physician or other healthcare provider if necessary.
Rest is required in the aftermath of an injury, and it cannot be overstated. Failure to provide the brain with adequate time for healing can lead to complications and cognitive impairment. As a result, it is critical to maintain a consistent amount of rest in order to promote brain healing as well as overall health.
The fact that prioritizing rest after a head injury has been shown to have positive outcomes in many cases is well documented in real-life examples and case studies. Rest, despite the fact that recovery varies by person, is still an essential component of healing.
As a brain recovery specialist, I strongly encourage individuals to be aware of the importance of good sleep and good rest habits in a brain recovery effort. Taking good care of your sleep hygiene, for example, can benefit your brain’s healing process.
Finally, let us keep in mind that our brains are remarkable organs that can heal and adapt to meet unforeseen challenges. As a result, by incorporating the importance of post-injury rest and taking proactive steps toward optimal recovery, we can empower our brains to recover stronger and stronger. Let’s prioritize rest, listen to our bodies, and make a plan for a fresh and revitalized brain. Our incredible minds, our incredible strength, and the power of recovery can all be harnessed by coming together.










